
In case of parametric mapping, not all software providers do have a specific tool. For LV volumetry and flow quantification, the contour relies on the definition of a whole pixel or subpixel depending on the software. Quantitative analysis is mostly based on manually contouring or manually correction of semi-automatic segmented regions of interest (ROI) in CMR images. They often differ within and between sites. CMR image analysis is performed on dedicated commercial and non-commercial software solutions. Interestingly, it is not suggested to report the software used. The Society for Cardiovascular Magnetic Resonance (SCMR) published not only standardized protocols for image acquisition and interpretation, but also guidelines for reporting which propose to report scanner type, sequences used and study quality. Technical aspects such as field strength, vendor platforms and imaging protocol influence CMR results. Therefore, accurate and reliable quantification is essential for correct diagnosis and adequate treatment. the placement of an implantable cardiac defibrillator depends on quantified LV function or valve replacement on quantitative flow assessment. Clinical decision-making is often based on quantification, i.e. In addition to mere functional assessment, non-invasive tissue differentiation represents CMR’s unique feature. CMR is the recommended method to assess cardiac function and hemodynamics especially when transthoracic echocardiography is limited. Due to its high accuracy and reproducibility, CMR is considered as gold standard for evaluation of left ventricular (LV) function. In the past years, cardiovascular magnetic resonance Imaging (CMR) has emerged as a broadly applied imaging modality in cardiac diagnostics. Registered 14 July 2017, retrospectively registered. CMR reports should contain the name and version of the software applied for image analysis to avoid misinterpretation upon follow-up and research examinations. In contrast to that, Vmax and T1-time may be influenced by software. Software had no impact on quantitative results of LV assessment, T2-time and SV based on 2D flow. For Vmax, equivalence was given between software A and C and for T1-time equivalence was given between software B and C. Differences between software were detected in flow measurement for Vmax and in parametric mapping for T1-time. All three software (A/B, A/C, B/C) were considered equivalent for LV EF, EDV, ESV, mass, 2D flow SV and T2-time. Resultsįor each parameter, thirty data sets could be analyzed with all three software.

Equivalence was considered if the confidence interval of a paired assessment of two sofware was within a tolerance interval defined by ☑.96 highest standard deviation obtained by intraobserver analysis. Forty-five data sets were evaluated twice (15 per software) for intraobserver analysis. Pixel-wise generated native T1- and T2-maps were used to assess T1- and T2-time. Phase-contrast magnetic resonance images were evaluated for forward stroke volume (SV) and peak velocity (Vmax).
Medis medical imaging systems free#
Cine steady state free precession short axis images were analyzed regarding LV ejection fraction (EF), end-systolic and end-diastolic volume (ESV, EDV) and LV mass.
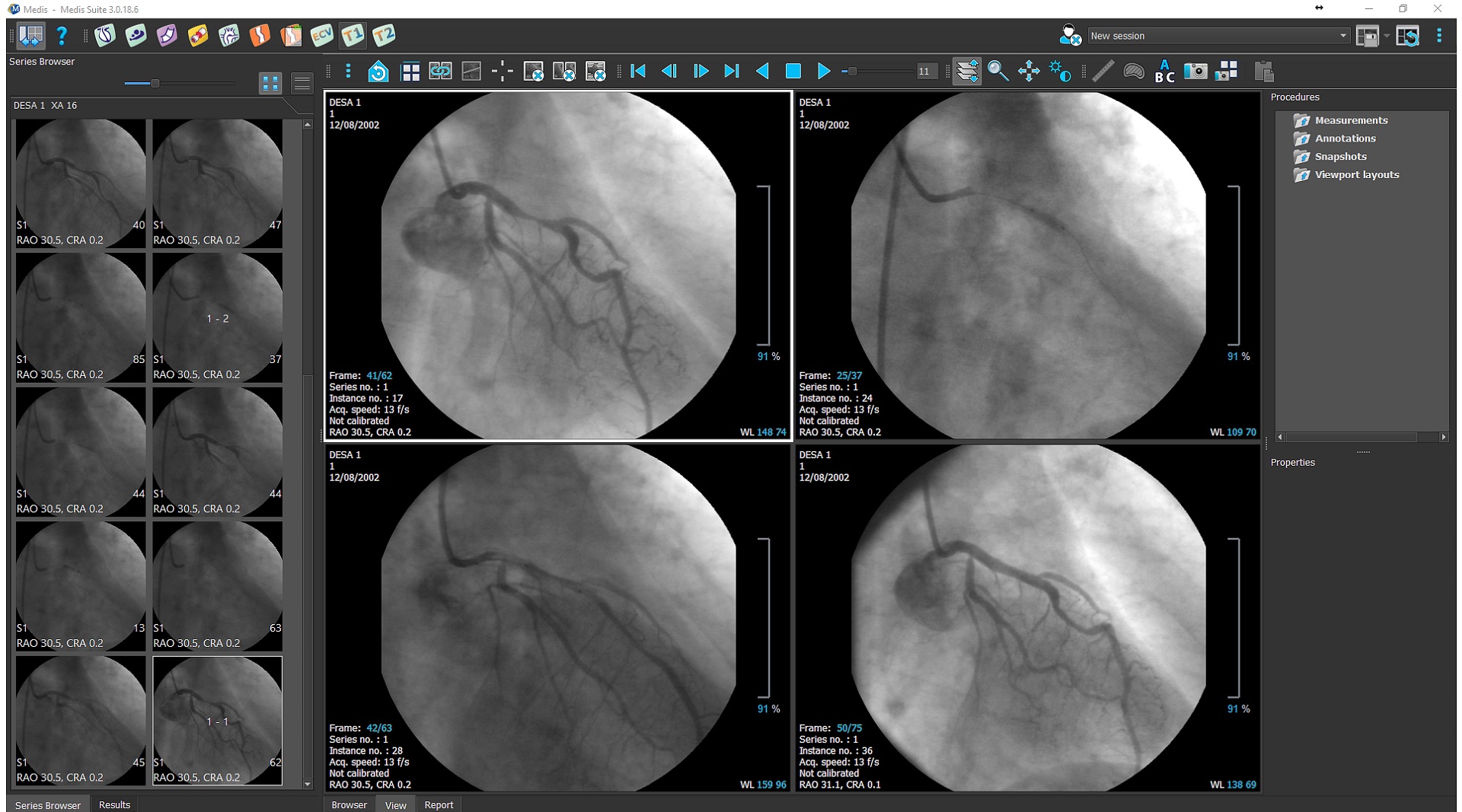
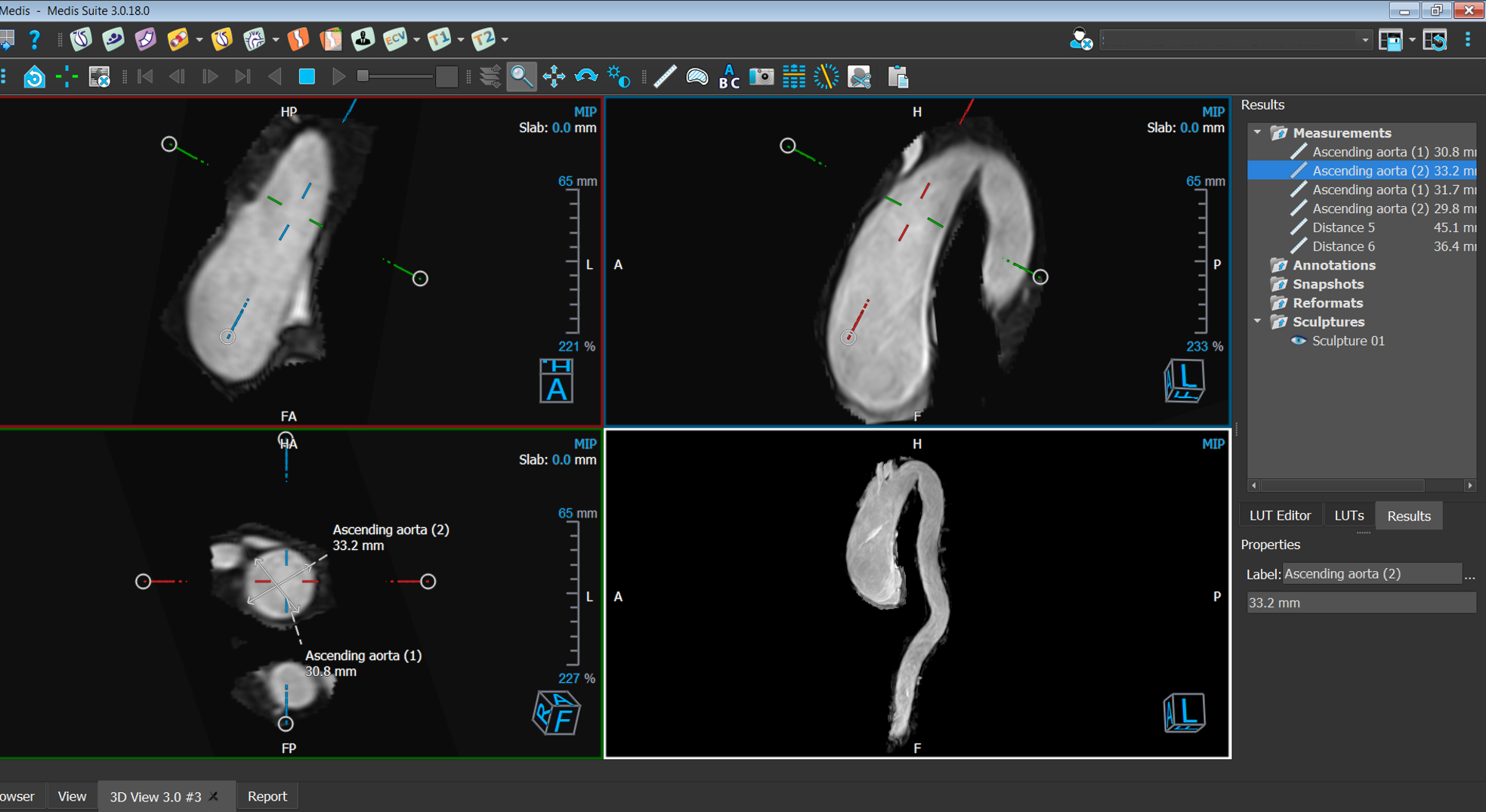
Thirty-one data sets of patients who underwent a CMR Scan on 1.5 T were analyzed using three different software (Circle CVI: cvi 42, Siemens Healthineers: Argus, Medis: Qmass/Qflow) by one reader blinded to former results. The aim of this study was to evaluate the impact of software on quantification of left ventricular (LV) assessment, 2D flow measurement and T1- and T2-parametric mapping. The manufacturers provide different analysis tools whose algorithms are often unknown. Image analysis is performed based on dedicated software. Quantitative results of cardiovascular magnetic resonance (CMR) image analysis influence clinical decision making.


 0 kommentar(er)
0 kommentar(er)
